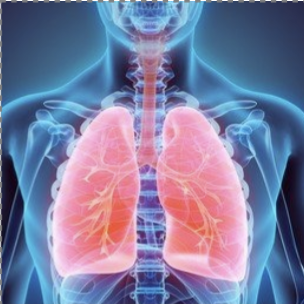
BACKGROUND: Acute respiratory distress syndrome (ARDS) is a result of diffuse lung injury and dysregulated inflammation. Recent studies have demonstrated that B cells can perform anti-inflammatory and tissue-protective functions. We hypothesized that systemic B-cell administration could have therapeutic effects in hyperoxic acute lung injury.
METHODS: Acute lung injury was modeled in adult C57BL/6J male mice through continuous exposure to hyperoxia (FiO2 >90%). Mature B cells (CD45R+/CD19+) were purified from spleens of age- and sex-matched C57BL/6J mice. B cells (107) or saline were administered intravenously after 24 hours of hyperoxia. Hyperoxia exposure was continued for up to 96 hours. The effects of adoptive B-cell therapy were assessed using histologic, physiologic (pulse oximetry, echocardiography), and immunologic (flow cytometry) readouts.
RESULTS: Hyperoxia led to a 50% depletion of endogenous pulmonary B cells by day 3, from 30% to 15% CD45+ lung immune cells (95% confidence interval [CI], 6.16-24.45; P = .0017). B-cell administration ameliorated B-cell loss, improved lung injury scores (median score in saline-treated = 3.0 vs B-cell-treated = 2.67; P = .0101) and lung cellular infiltration (F [2,34] = 11.99; P = .0001). By day 3, B cells limited the duration of oxygen desaturations (difference 0.39 seconds; median length = 1.01 seconds in saline-treated vs 0.62 seconds in B-cell-treated; 95% CI, 0.02-0.73 seconds; P = .03) and their depth (median nadir = 82.0% in saline-treated vs 85.9% in B-cell-treated, 95% CI, -6.6% to -0.84%; P = .04). B-cell-treated mice showed a median 3.82% increase in left ventricular ejection fraction by day 3, compared to 12.35% in saline-treated mice (mean difference 7.32%; 95% CI, -5.0% to 19.6%; P = .23). Exogenous B cells represented less than 1.5% of pulmonary B cells on day 3. B-cell administration had homeostatic effects on relative abundance of pulmonary immune subsets affected by hyperoxia, including endogenous B cells, CD4+ T cells, natural killer (NK) cells, monocytes/macrophages, and neutrophils. Significant immunomodulatory effects of B-cell administration were observed in myeloid cells in the lungs and included reductions in the proportion of interleukin-17 (IL-17)-expressing Ly6Clo monocytes (F [2,14] = 19.02; P = .0001), alveolar macrophages (F [2,14] = 10.32; P = .0018), and neutrophils (F [2,14] = 6.621; P = .0095) as well as interferon-gamma (IFNγ)-expressing Ly6Clo monocytes (F [2,14] = 48.83; P = .0001).
CONCLUSIONS: Our data indicate that adoptive B-cell therapy ameliorates hyperoxic lung injury and may represent a novel treatment for ARDS.