This is the first of what will be regular progress updates on the Project SUCCESS website. Since the project started in January 2020, we’ll begin by reviewing what we’ve been doing since then.
We were fortunate to have been able to bring together a great team of leading clinical researchers and experts on our interventions to help us develop and implement the project.
CET experts
-
Shaun M. Eack, PhD, University of Pittsburgh.
-
Maralee Litschge, LCSW, University of Pittsburgh
HOPES experts
-
Kim T. Mueser, PhD, Boston University
-
Sarah I. Pratt, PhD, Dartmouth Hitchcock Medical Center
-
Meghan Santos, MSW, Dartmouth Hitchcock Medical Center
Neurocognitive expert
-
Raquelle Mesholam-Gately, PhD, Beth Israel Deaconess Medical Center
Biostatistics expert
-
Haiyi Xie, PhD, Dartmouth College
We began meeting with this co-investigator team as soon as we received the PCORI funding. We also visited principal investigators at the sites that had agreed to provide one of the two treatments in Project SUCCESS and began to hire study staff, starting with Matt Killam, our Research Coordinator (subsequently promoted to Clinical Trials Specialist). Then, in March 2020, the COVID-19 pandemic struck.
For the rest of 2020, we worked with PCORI to design a plan for continuing the project in a way that would be feasible despite the complications caused by the pandemic and the shift to remote delivery of many mental health services. In 2021, we conducted a pilot study of the feasibility and acceptability of remote delivery of both of our treatments. Four of our treatment sites participated in this pilot, with two delivering CET and two delivering HOPES, and one of the two providing the assigned treatment in person and the others providing the assigned treatment virtually. All research assessments were administered through the web, with Zoom or Teams.
The pilot phase at each of the four sites concluded after three months, although research and treatment then continued at each of these sites for the full 12 months (with additional research assessments administered 6 and 12 months after treatment completion). We spent all of 2021 carrying out the pilot phase at the four sites. By the end of 2021, our pilot experience and satisfaction surveys of participants had demonstrated that we could deliver the treatment remotely and that this approach was as acceptable to participants as in person delivery.
The pandemic was subsiding as we finished our pilot project, so in 2022 we prepared to launch the full project with in-person treatment delivery at all sites. Although our pilot had demonstrated feasibility and acceptability of remote treatment delivery, the brief pilot could not test the effectiveness of this modality. We were relieved that we could use the tried-and-true method of in-person group sessions for both treatments (some sites conduct individual sessions remotely).
The pandemic was followed by staffing shortages at many mental health service centers and as a result we had to replace some sites that no longer had sufficient clinical staff to deliver our treatments. By the end of 2022, we had our final roster of sites and the first one had begun to deliver treatment. Throughout 2023, we have continued to launch treatment sites, work with sites to recruit and assess participants, and monitor treatment delivery.
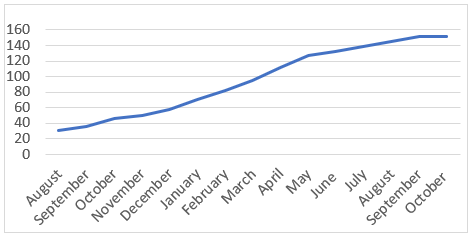
At present, we are working with 13 different mental health service sites. Figure 1 displays the pace of recruitment as we move close to full enrollment.
Figure 1
Enrollment in Project SUCCESS
To October 2023
Clinicians at our participating sites are now delivering CET or HOPES to 16 treatment groups. Although outcome data will not be available until the conclusion of the project, we conduct qualitative interviews with a randomly selected half of treatment participants to learn about their experiences. Figure 2 displays some of their comments.
Figure 2
Selected Participant Comments about Group Experience
Qualitative Interviews of Randomly Selected Participants before October 2023
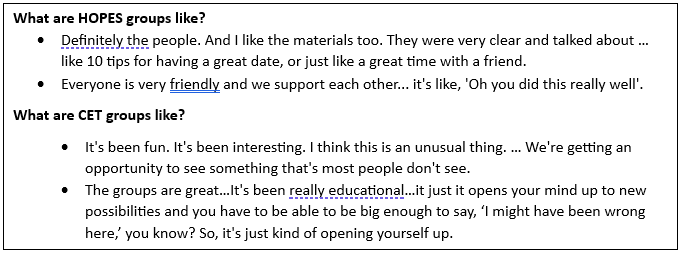
You can see why we think Project SUCCESS is succeeding!
Russ and Kesh
Russell K. Schutt, PhD and Matcheri S. Keshavan, MD, Beth Israel Deaconess Medical Center
