Acute pancreatitis may be the initial clinical presentation of pancreatic cancer. However, since the vast majority (approximately 98%) of acute pancreatitis is due to other causes (e.g. alcohol, gallstones), pancreatic cancer is generally not pursued as a possible etiology unless a mass is observable. Therefore, cases of pancreatic cancer may be missed in the early stages.
We postulated that patients with acute pancreatitis confined to the body and tail of the pancreas with sparing of the head may be due to small tumors obstructing the pancreatic duct.
We designed a retrospective chart review study of all patients in a two-year period with newly diagnosed acute pancreatitis. Patients with known identifiable causes (including pancreatic cancer, a visible mass, history of prior acute pancreatitis, sequela of necrotizing acute pancreatitis, and prior pancreaticobiliary intervention) were excluded. The remaining were evaluated for the presence of isolated distal pancreatitis as seen on CT.
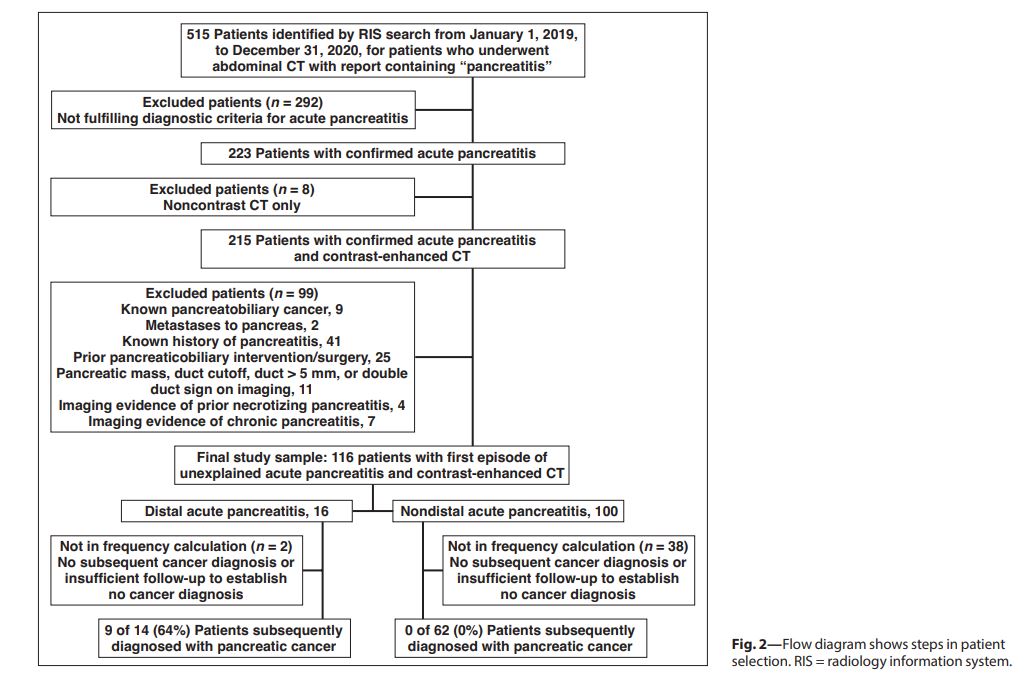
Although isolated distal pancreatitis is a small percentage of total acute pancreatitis, within that group, about half were subsequently diagnosed with pancreatic cancer.
The recognition of isolated distal pancreatitis in the absence of an identifiable cause as a potential harbinger of pancreatic cancer provides an opportunity to identify and provide treatment for a subset of pancreatic cancer patients months or years before they might otherwise be diagnosed.
To learn more, view our published AJR paper, "Unexplained Acute Distal Pancreatitis: Association With Subsequent Diagnosis of Pancreatic Cancer."
