Lymphedema is caused by the accumulation of lymphatic fluid in the interstitial space due to impaired clearance, from congenital causes (primary) or infection, trauma, or medical/surgical treatments (secondary), resulting in (sometimes severe) swelling of the extremities.
Visualization and characterization of areas of edema are necessary to better plan interventions and to further study the pathophysiology associated with lymphedema. The standard methodology for the evaluation of lymphedema involves the injection of contrast agents with optical imaging or ultrasound; both visualize only the superficial lymphatic vessels and areas of edema.
We have been developing Magnetic Resonance Imaging (MRI) as a noninvasive, more complete, and potentially more sensitive method for the evaluation of lymphedema.
We first demonstrated a system of staging lymphedema from standard MRI scans. Given that MRI can visualize the arm along its full length and in its entire cross-section, the staging was based on the degree of circumferential subcutaneous fluid infiltration seen along the epifascial regions or infiltrating the subcutaneous fat, evaluated at three points: the elbow, upper arm, and forearm. The figure at the bottom of the page shows one example case of stage 1 lymphedema in a woman with a history of breast cancer treatment; the fluid (yellow arrows and shading) is along the forearm and elbow, without infiltration at the upper arm.
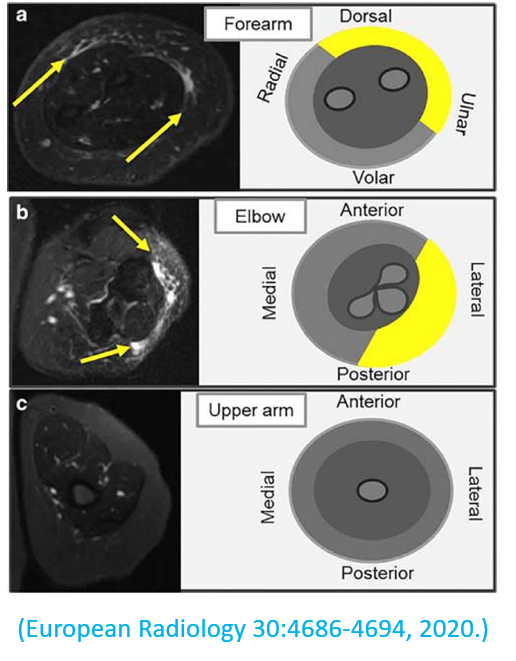
Higher MRI staging correlated with abnormal standard measurements such as backflow on lymphoscintigraphy or abnormal lymphography patterns, but also enabled evaluation of the full anatomic patterns of the edema, as demonstrated in the next study.
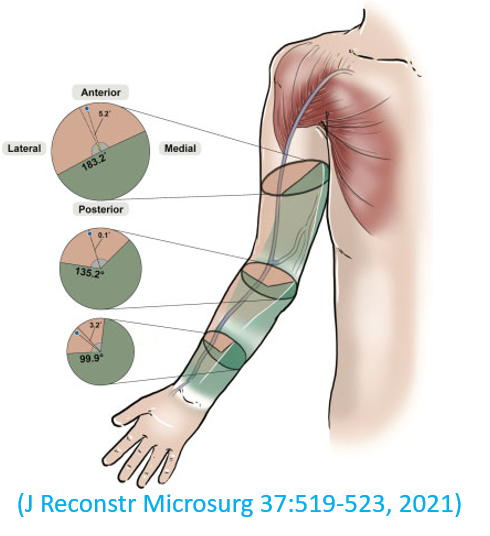
With MRI, we demonstrated that areas of edema sparing, when present, were centered around the cephalic vein as shown in the schematic on the right. This may be explained by the presence of the Mascagni-Sappey (M-S) lymphatic pathway as it is located alongside the cephalic vein and motivates additional research to better elucidate any trends between the presence of the M-S pathway, areas of sparing, and severity of lymphedema.
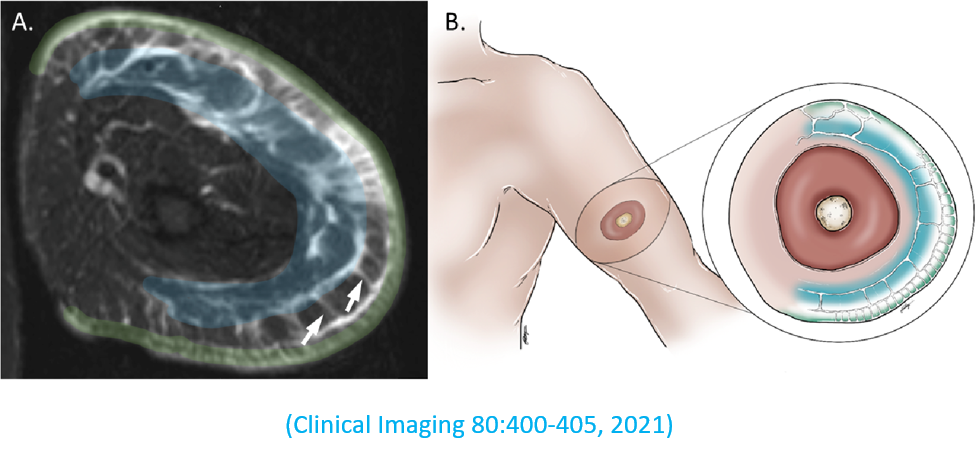
Following up on our initial study, we described a specific combination of signs, which we refer to as the “dermal rim sign”, as being indicative of lymphedema severity and potentially useful as a diagnostic biomarker. The combination of signs consists of “honeycombing”, hyperintense signal of the overlying thickened skin, and fluid signal in the subcutaneous tissue (see image).
Together, these findings demonstrate the potential for MRI as a sensitive, specific, and noninvasive modality for diagnostic and therapeutic planning in lymphedema, as well as opening the door to understanding this debilitating condition and the development of new therapeutic approaches.
Additional References
- Kim G, Adondakis M, Smith MP, Singhal D, Tsai LL. Rate of Incidental Edema in the Contralateral Arm of Patients with Unilateral Postsurgical Secondary Upper Extremity Lymphedema. Lymphat Res Biol. 2023 Apr;21(2):111-117. PMID: 35914097. PMCID: PMC10325808. https://doi.org/10.1089/lrb.2021.0022. Epub 2022 Aug 01.
- Friedman R, Lee C, Kinney JR, Salehi BP, Kim G, Singhal D, Tsai LL. Fluid Distribution Patterns in Early-Stage Upper Extremity Lymphedema. Ann Plast Surg. 2023 Jun 1;90(6S Suppl 5):S622-S625. PMID: 37399485. PMCID: PMC10318265. https://doi.org/10.1097/SAP.0000000000003494. Epub 2023 Feb 18.
- Kinney JR, Babapour S, Kim E, Friedman R, Singhal D, Lee BT, Tsai LL. Edematous Dermal Thickening on Magnetic Resonance Imaging as a Biomarker for Lymphatic Surgical Outcomes. Medicina (Kaunas). 2023 Jul 26;59(8):1369. PMID: 37629659. PMCID: PMC10456688. https://doi.org/10.3390/medicina59081369. Epub 2023 Jul 26.
- Kim C, Ali H, Tsai LL, Bulman J, Singhal D, Carroll B, Ahmed M, Weinstein J. Evaluation of Primary Lymphedema with Intranodal Lymphangiography. Cardiovasc Intervent Radiol. 2023 Nov 20. PMID: 37985479. https://doi.org/10.1007/s00270-023-03605-9. Epub 2023 Nov 20.
