Interventional Radiology (IR) is rapidly increasing in terms of the types of procedures and the volume of cases. The growth of this field is evidenced by the new residency training program for this specialty.
As IR requires proficient technical skills in interventions, assessment of those skills is important for both training purposes (e.g. feedback to the trainee) and assessment of technical competency.
We implemented an electromagnetic hand motion tracking system to determine if it could detect the small motions associated with IR procedures, and differentiate between levels of expertise as a first step in assessing the potential of this technology for training and evaluation within IR.

A sensor was placed on the dorsum of the hand. Two tasks were utilized to assess the tracking system; a “sheath task” in which participants were asked to thread a wire through the opening of a sheath, and then “pin-pull” the dilator of the sheath over the wire, and a radial artery access task implemented in a mannequin arm with a pneumatic pump to simulate arterial pulsation.
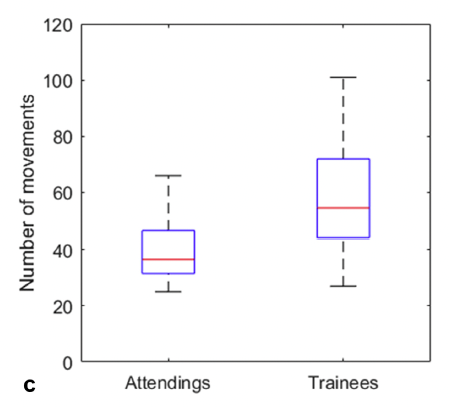
The time, path length, and number of movements were all lower for experienced attendings as compared with trainees, demonstrating the sensitivity of the system to motions associated with the IR procedures and the ability to differentiate the motions of experts versus trainees.
This ‘proof of principle’ study enabled several investigations into aspects of the technical proficiency of IR procedures and methods for improvement.
Identifying areas for training focus:
In the first study, a mannequin was used to simulate central line placement. Sensors on the ultrasound probe and needle hand were used to analyze the motions of those aspects of the line placement.
The results demonstrated that the metrics for the probe motion were different for junior and senior trainees, demonstrating improvement in this aspect of the procedure during residency. However, that was not the case for the needle hand motion, where no difference was found between junior and senior trainees (and both being different than the motion of experts). These results suggest that further attention be paid to training the needle movements during training. (ref abstract)
Identifying methodologies for improved training:
In the second study, simulations of central line placement were again used, this time to investigate feedback to the trainees based on motion metrics versus traditional feedback.
For the traditional feedback group, scores were not different between the first and last trials. In comparison, participants in the motion-based feedback group significantly improved, suggesting a larger place for motion-based feedback in residency training programs. (ref abstract)
These studies provide clear and quantitative findings to best train and evaluate future clinicians, supporting this new and rapidly expanding field of interventional radiology.
