Variable Anatomy & Function
Extramural funding: 5R01HL157991-05 Variable Anatomy & Function
of the Arm's Alternate Lymphatic Pathway
Breast Cancer-Related Lymphedema (BCRL)
Breast cancer related lymphedema affects 1.2 million patients in the U.S. and is one of the most significant cancer survivorship burdens. Lymphedema can develop following the removal of lymph nodes during an axillary lymph node dissection, a procedure performed during breast cancer treatment.
Anatomy
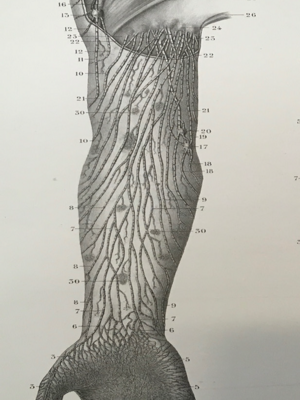
The main lymphatic channels, or pathways, of the arm terminate in the axilla and would be disrupted during an axillary lymph node dissection (ALND).
However, secondary or collateral pathways have also been described which variably terminate in the axilla or drainage basins outside the axilla (e.g. supraclavicular nodes). These would be spared during an ALND.
Secondary pathways act as a back-up pathway for the drainage of the arm, especially in the event of damage to the primary drainage pathway.
A breast cancer patient will experience a “double hit” if they undergo an ALND and subsequent surgical disruption or radiation injury to these secondary pathways during breast cancer treatment. The “double hit” could predispose patients to post-operative lymphedema.
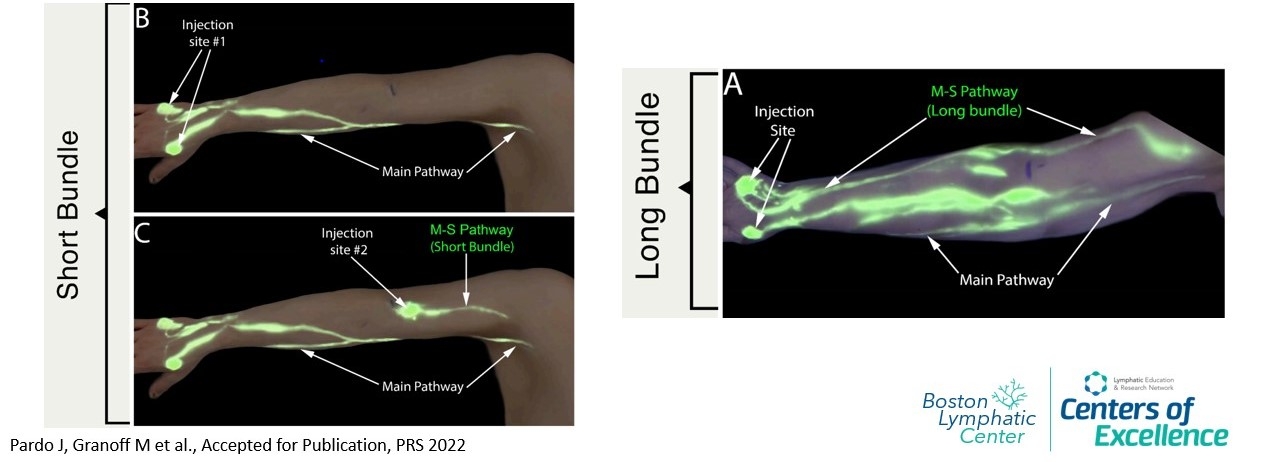
The M-S Pathway
The main secondary pathway of the arm was originally described by anatomists Mascagni in 1787 and by Sappey in 1874. Termed the Mascagni-Sappey (M-S) pathway, anatomists Kubik and Leduc in the 1900s clarified its presence in the posterior upper arm adjacent to the cephalic vein.
The M-S pathway has been described as a “compensatory” pathway for lymphatic drainage of the limb, underscoring its importance in patients who have damage to their main drainage pathways after ALND or radiation.
Our Study
This NIH-funded study (project number 5R01HL157991-05 funded by NHLBI of NIH) aims to identify normal variations in lymphatic anatomy (different arrangements of vessels or pathways through which excess fluid travels) and function of the upper extremities that may predispose women to lymphedema.
Specifically, this study has two primary aims:
| Aim 1 | Aim 2 |
|---|---|
| Define an alternative lymphatic route, the M-S pathway in the upper extremity of healthy female volunteers. | Define the M-S pathway anatomy after axillary lymph node dissection (ALND) surgery in breast cancer patients without lymphedema. |
| These volunteers do not have a history of lymphedema or ALND surgery. | These volunteers are at least 2 years post ALND surgery and have not developed lymphedema. |
| We hope to quantify the percentage of women who do not have the M-S pathway present, do not have peripheral connections between the M-S pathway and the forearm, and/or whose terminal MS pathway draining nodal basins are in the axilla. | Examining the M-S pathway anatomy in the setting of an ALND without lymphedema allows us to gain critical insight about which patients are at the highest risk of developing breast cancer-related lymphedema |
| We hypothesize that we will see significant variability in the M-S pathway in our Aim 1 volunteers. | We hypothesize that the M-S pathway becomes the dominant lymphatic drainage pathway of the upper extremity after ALND in patients who do not develop lymphedema. |
Despite the potential importance of these pathways, no prior attempts have been made outside the anatomy laboratory to clinically map and study the normal variations of the M-S pathway (Aim 1). Moreover, no study has been undertaken to understand how these pathways are altered after cancer therapy such as an axillary lymph node dissection (Aim 2). We aim to address these deficiencies through the proposed research study.
Study Procedures
To test these hypotheses, we perform indocyanine green (ICG) lymphography and lymphoscintigraphy scans of the bilateral upper arms of our volunteers to evaluate the anatomy of the M-S pathway.
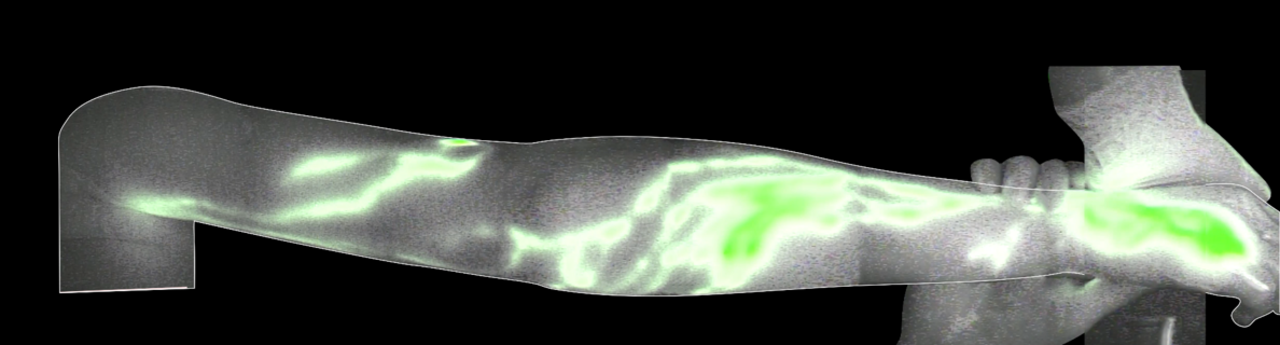
ICG Lymphography: This exam uses a combination of dye called indocyanine green (ICG) that glows at certain wavelengths and a special camera that can capture images and video illuminated by the dye. This method is used to visualize lymphatic shallow vessels underneath the skin.
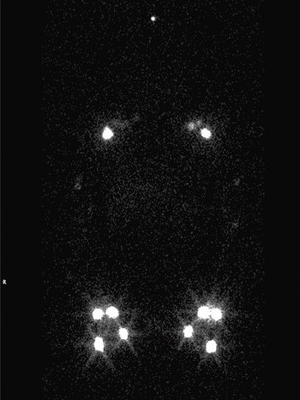
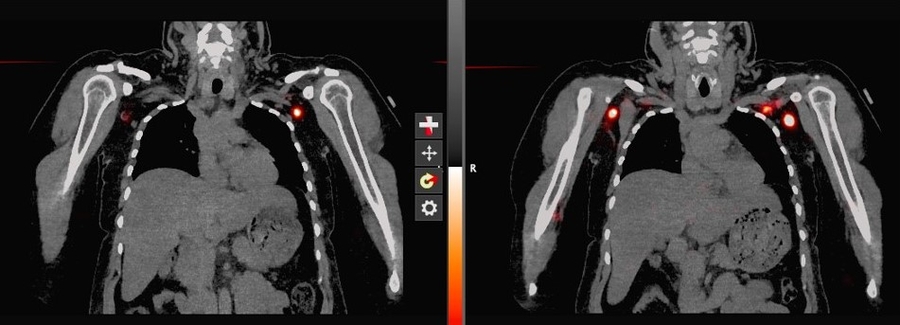
SPECT/CT Lymphoscintigraphy: SPECT/CT stands for single-photon-emission computed tomography. This scan consists of combining a CT scan (which lets us see your anatomy clearly) with a scan that tracks the progression of a tracer through that anatomy over a certain period of time. It lets us see the volunteer's anatomy with clarity as the tracer moves through.

